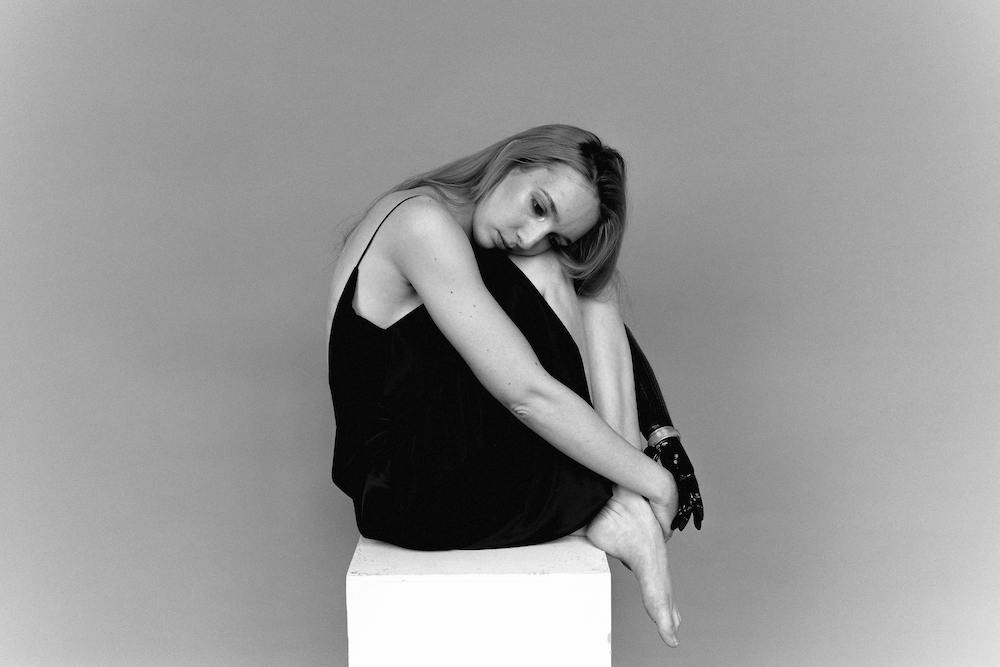
13 May Is it Postpartum Depression or the Baby Blues?
Feeling down after giving birth? The hormonal fluctuations after giving birth can be a crazy ride because of the rapid drop in estrogen and progesterone that supported your pregnancy. Now that your baby is born, the high levels of these hormones are no longer needed. This phenomenon can lead to the Baby Blues, which affects 85% of postpartum women.²
The Baby Blues are characterized by feeling sad, anxious or overwhelmed in the first couple of weeks postpartum. You might have crying spells, a loss of appetite, or difficulty sleeping. These symptoms of depression are mild, however, and usually don’t impair your overall functioning. Typically, these feelings resolve in a few days and no medical intervention or treatment is needed. Your hormones rebalance and life goes on with healthy mother/baby bonding and appropriate integration of your new baby into the family.
Postpartum depression (PPD) is a different phenomenon. The symptoms of postpartum depression are more intense and pervasive. Feelings of sadness are profound and mood swings can be severe. Symptoms that begin like the Baby Blues persist past the first few weeks. Prolonged, untreated symptoms can eventually impair a mother’s ability to care for herself and her baby.
PPD affects mothers of all races and cultures, although the condition may manifest differently due to social conditioning. Key features include irritability and rejection of the baby. Irritability can flare into angry outbursts or dissolve into crying. A mother may act disinterested, annoyed, or jealous of the baby. She may blame the baby for a lack of maternal feelings. She may have thoughts of harming her baby. These thoughts and behavior may, in turn, elicit feelings of fear, shame and guilt.²
What are the Risk Factors for Postpartum Depression?
Risk factors for postpartum depression are multifactorial. This means hormonal changes, mental health history and situational factors often all play a role. Precipitating factors can include:
- maternal anxiety and depression before or during pregnancy
- life stressors
- poor relationship quality
- intimate partner violence
- low income
- unintended pregnancy
- single motherhood
- lack of social support
- traumatic birth experience
- preterm infant
- multiples
- breastfeeding problems
- thyroid imbalance.¹
Postpartum depression rarely gets better without intervention. Oftentimes, a holistic approach is needed that includes antidepressant medications, psychotherapy, and a social support network. Many mothers include supportive, integrative therapies into their treatment plan, like massage, acupuncture, and mindfulness meditation, which cultivate feelings of wellbeing.
If you are experiencing any of the above mentioned symptoms, don’t despair. The first step is making an appointment with your healthcare provider. Take the Mommyato Brain Power Assessment to help screen for postpartum depression. If you are having frightening thoughts of harming yourself or your baby, go immediately to the emergency room for medical care. To find support and resources in your area, check out the National Institute of Child and Maternal Health site funded by the U.S. Department of Health and Human Services.
Help is available. Reach out and tell someone what you are going through. You are not alone!
REFERENCES:
- American College of Obstetricians and Gynecologists (ACOG). (2018). Screening for perinatal depression. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/11/screening-for-perinatal-depression
- Lowdermilk et al. (2016). Maternity and women’s health care. Elsevier Inc
- Photo by Anna Shvets: Woman Sitting While Looking Lonely. https://www.pexels.com/photo/woman-sitting-while-looking-lonely-3732640/